The Lipedema Guide
A blueprint for lowering inflammation, supporting lymphatic and vascular function, restoring micronutrient balance, and reducing immune load
If you are reading this, you have likely already encountered my previous Substack article on lipedema, where I reviewed what the research is consistently showing at diagnosis.
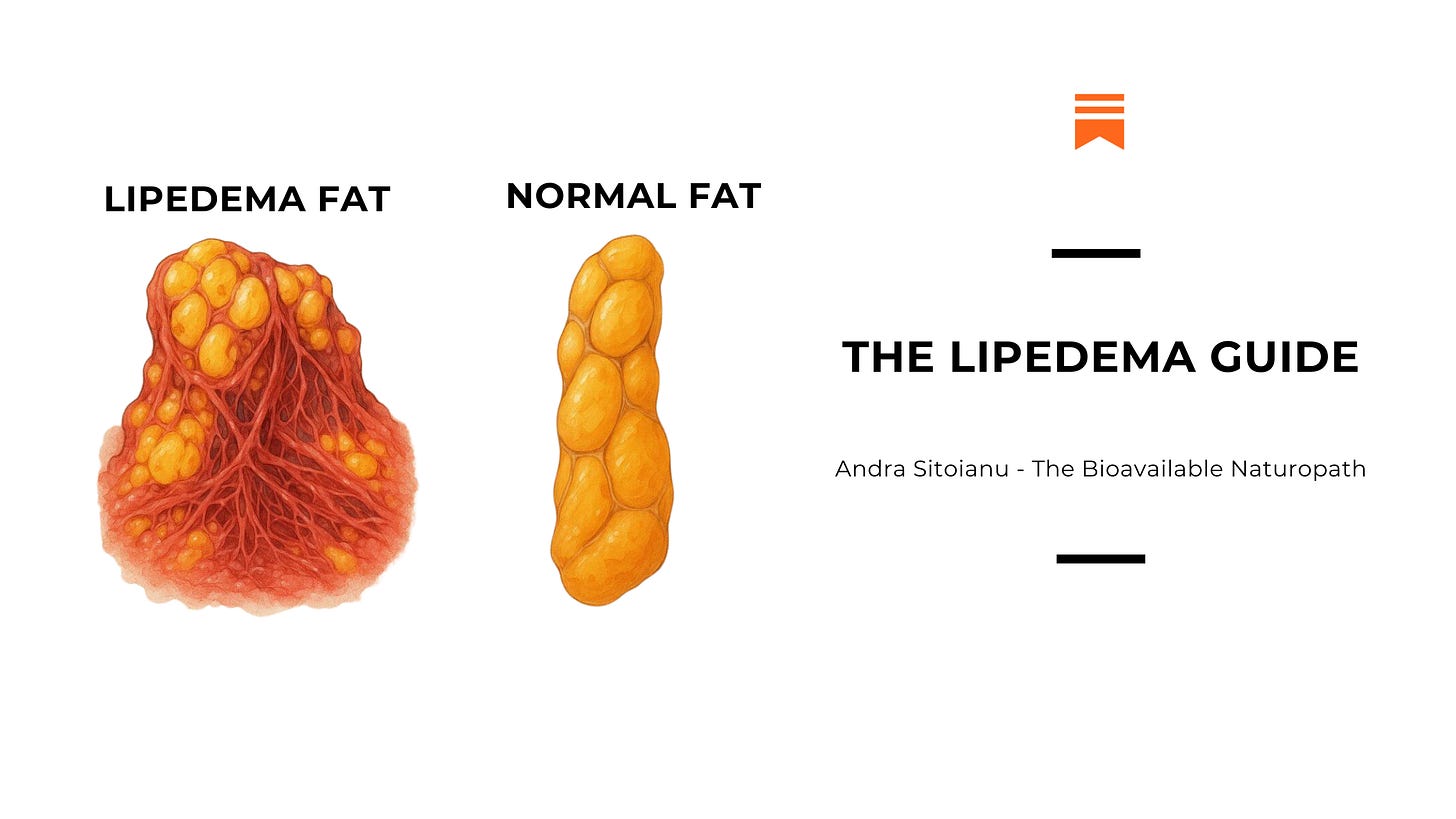
To briefly recap, large clinical cohorts of people with lipedema demonstrate striking patterns long before any intervention begins. These include extremely high rates of suspected gut permeability, frequent thyroid abnormalities most often thyroid nodules, ovarian and hormonal dysfunction, widespread joint hypermobility, mast cell activation and histamine intolerance, and a surprisingly high prevalence of nickel allergy and immune hypersensitivity.
These findings matter because they show that lipedema does not develop in isolation. It emerges in a system already under immune, inflammatory, hormonal, and lymphatic load.
Since publishing that article, additional data has strengthened this picture. Selenium deficiency has been documented in a large proportion of patients with lipedema and related lymphatic disorders, pointing to impaired antioxidant and immune regulation. Lactoferrin has also gained relevance due to its role in immune modulation, gut barrier integrity, and reduction of inflammatory and microbial signaling.
Together, these findings reinforce a core principle. Lipedema support works best when it focuses on regulation, not force.
What Is Biologically Modifiable in Lipedema
Lipedema does not respond predictably to calorie restriction or exercise because it is not driven by energy balance alone. It reflects how tissue behaves in response to signaling from the immune system, the gut, hormones, blood vessels, lymphatic flow, and the nervous system.
Clinical experience and research converge on six biological levers that consistently shape symptom expression.
Lipedema support is most effective when it:
lowers inflammatory signalling
reduces immune and mast cell activation
restores gut barrier integrity
improves hormonal processing
reduces vascular leakiness
improves tissue comfort and tolerance
Each of these levers influences pain, swelling, bruising, fatigue, and flare frequency. Addressing them together changes how the tissue behaves, even when structural change is slow.
Nutrition and Lifestyle as Regulatory Tools
Nutrition and lifestyle influence every modifiable lever in lipedema.
A supportive dietary pattern emphasizes:
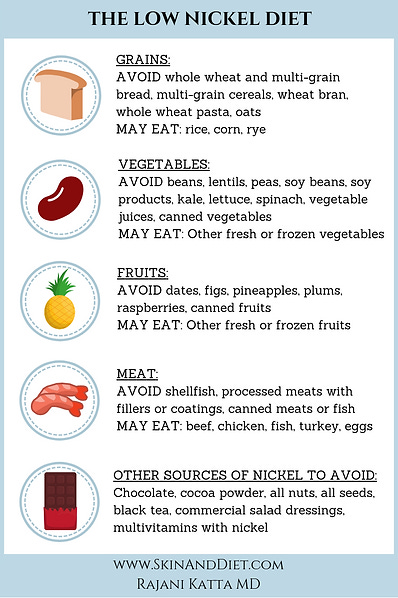
low nickel intake to reduce immune hypersensitivity, 60% of lipedema tested positive for nickel allergy
A low nickel diet is quite low in inflammation regardless of the sensitivity: minimal grains, no soy, no canned or processed foods.
A low nickel diet is also low in estrogenic mycotoxin releasing mold prone foods like grains, peanuts, nuts.
adequate choline for estrogen metabolism and cell membrane integrity, enjoy pasture raised chicken egg yolks bountifully.
gelatine and collagen-rich foods for gut and connective tissue support: meat broths, gelatine based gummies.
blood sugar needs to be stabilized:
glucose tolerance follows a circadian pattern, with greater insulin sensitivity earlier in the day and reduced tolerance in the evening. Aligning meal timing with this rhythm supports metabolic efficiency and reduces glycemic stress on lipedema-affected tissues. Regular meal timing anchors circadian signalling and stabilizes insulin release. Consuming balanced meals with protein, gentle fibre and healthy saturated fats earlier in the day, supports steady blood sugar levels and reduces compensatory hormonal responses later in the evening.
fruit-forward carbohydrates to support vitamin C and antioxidant intake, metabolism, CO₂ production, support histamine breakdown and lymphatic flow: pomegranates, berries, melons, ripe fruit available locally: cooked and stew fruit in the winter is wonderful way of enjoying fruits in the cold season.
Lifestyle strategies that support regulation include gentle movement, compression socks, stress reduction, and reducing exposure to estrogenic pesticides, mold-related mycotoxins, plasticizers, and heavy metals.
Gentle Movement and Lymphatic Circulation
Movement supports lymphatic circulation through rhythmic muscle contraction and joint motion. In lipedema, tissues benefit from forms of movement that encourage steady fluid transport while preserving connective tissue integrity. Walking, swimming, rebounding at a comfortable pace, Pilates, and slow strength-based practices promote lymph flow and circulation.
Daily movement supports glucose uptake by skeletal muscle, improves mitochondrial efficiency, and reduces postprandial blood sugar variability. Short, regular sessions reinforce metabolic signaling without provoking stress responses.
Compression as Structural Support
Graduated compression garments provide external support to tissues that experience altered fluid dynamics. Compression enhances venous and lymphatic return, reduces interstitial fluid accumulation, and improves proprioceptive feedback. These mechanical inputs contribute to tissue stability and comfort throughout the day.
Regular daytime use during periods of activity or prolonged sitting supports fluid balance and reinforces vascular rhythm.
Stress Reduction and Nervous System Regulation
The nervous system plays a central role in blood sugar regulation through its influence on cortisol, insulin sensitivity, and vascular tone. Chronic stress alters these pathways and increases metabolic variability across the day.
Supporting parasympathetic activity through regular sleep timing, exposure to morning light, paced breathing, and gentle evening routines improves coordination between the brain, endocrine system, and peripheral tissues. A regulated nervous system supports more predictable glucose handling and reduces inflammatory signaling.
Blood Sugar Regulation Aligned With Circadian Rhythm
Morning light exposure further synchronizes central and peripheral clocks, enhancing insulin sensitivity and cortisol rhythm. Evening light reduction supports melatonin secretion and overnight metabolic recovery. Chronic exposure to blue light when is dark outside will also increase insulin resistance, creating inorganic spikes that will drip into inflammatory cascades. The importance of light cannot be underestimated.
Environmental Estrogenic Exposures
Environmental exposure plays a meaningful role in lipedema because affected tissue is sensitive to hormonal signaling, immune activation, and oxidative stress. Certain environmental compounds interact directly with estrogen receptors, immune cells, and inflammatory pathways. Over time, this adds to the physiological load the body is managing.
Reducing exposure does not require perfection. Small, consistent changes lower background signalling and support better regulation across multiple systems.
Estrogenic Pesticides
Many agricultural pesticides interact with estrogen receptors or influence hormone metabolism. Chronic low-level exposure increases estrogenic signaling and immune activation within sensitive tissues.
In lipedema, where estrogen responsiveness is already heightened, this added signaling can:
increase tissue reactivity
worsen swelling and tenderness
amplify inflammatory and mast cell responses
Practical ways to reduce exposure include:
prioritizing organic produce when possible
washing and peeling conventionally grown fruits and vegetables
Effective way of removing pesticides with Baking Soda.
Mold-Related Mycotoxins
Certain molds produce mycotoxins that influence immune function, inflammation, and hormonal signalling. Some mycotoxins interact with estrogen receptors or disrupt hormone metabolism.
Chronic exposure to mold and damp environments is associated with:
immune dysregulation
increased inflammatory signaling
mast cell activation
hormonal disruption
In people with lipedema, this exposure can contribute to flare intensity and symptom persistence.
Supportive steps include:
addressing visible mold or water damage
improving ventilation and indoor air quality
avoiding damp living spaces
investigating ongoing musty odors
reduce exposre to moldy foods: grains, peanuts, nuts, beans are the major contributors, these are also highest in nickel.
Reducing mold exposure lowers both immune and estrogenic load.
Plasticizers and Synthetic Chemicals
Plasticizers such as phthalates and bisphenols are used in food packaging, personal care products, and household items. These compounds can interfere with hormone signaling and immune regulation.
Exposure occurs through:
food stored or heated in plastic
plastic bottles and containers
personal care products
household cleaning agents
These chemicals are associated with:
altered estrogen signaling
increased oxidative stress
immune activation
Simple exposure-reducing steps include:
storing food in glass or stainless steel
avoiding heating food in plastic
choosing fragrance-free personal care products
reducing use of synthetic household cleaners
Lowering plastic exposure reduces chronic endocrine and immune stress.
Heavy Metals With Hormonal and Immune Effects
Certain heavy metals interact with estrogen receptors, immune cells, and antioxidant systems. Over time, exposure contributes to oxidative stress and inflammatory signaling.
Common sources include:
contaminated water
older plumbing
cookware and food contact materials
environmental pollution
Reducing exposure may include:
using filtered drinking water
choosing safer cookware
being mindful of occupational or environmental exposure sources
verifying that dental devices like mercury amalgams, braces with nickel are not creating more havoc
Lower heavy metal exposure supports antioxidant balance and immune regulation.
Lipedema tissue responds strongly to cumulative signalling. Estrogenic compounds, immune disruptors, and oxidative stressors all add to the internal environment that tissue is reacting to.
Reducing environmental load:
lowers inflammatory signalling
reduces immune and mast cell activation
supports hormonal processing
improves tissue tolerance
These changes do not act on fat tissue directly. They improve the regulatory environment the tissue exists within.
Consistency creates cumulative benefit.
Helpful Labs
Keep reading with a 7-day free trial
Subscribe to The Bioavailable Naturopath to keep reading this post and get 7 days of free access to the full post archives.